Research can make a difference
See our research news
Outcome Health’s research platform, Aurora, provides an ethics-based ecosystem to engage in research by utilising de-identified data from participating GP practices.
PHNs have ownership and oversight of the de-identified data sourced from constituent practices and must consent to any data release. Aurora advocates for translational research with tangible benefit to PHNs, GPs and our communities.

Scaled national coverage
In partnership with PHNs, Aurora holds one of the few comprehensive general practice datasets in Australia. The dataset consists of privacy-protected, de-identified electronic medical records, extracted from thousands of participating practices across Australia.

Not for Profit
At Outcome Health, our independent governance framework ensures data is only provided for research activities with a clearly articulated translational plan to improve health outcomes in Australia. Under our governance model data is released only with PHN consent and is never shared commercially or for profit-based motives.

Ethics approval by the RACGP
Research conducted on Aurora data is covered by ethics approval.
Since August 2017, POLAR maintains ethics approval granted by the RACGP National Research and Evaluation Ethics Committee, for the collection, storage, and transfer of general practice data.
Projects must undergo individual ethics review prior to data sharing.

Apply for access
Researchers can apply for data access directly to PHNs or they can approach Outcome Health for any research queries. Final access approval for any subsets of de-identified general practice data, will be granted under PHN consent. For more information on the approval process, please contact Outcome Health via research@outcomehealth.org.au.
Current POLAR research projects
PHNs involved with Aurora have high exposure and engagement with research activity and can drive evidence-based change in their local areas. This section lists current projects. For an exhaustive list of completed projects, please email research@outcomehealth.org.au.
COVID-19 – Policy and Evidence (Phase II)
The interruption of normal patterns of health care and the suspension of services during COVID-19 has meant that the pandemic has also had a major impact on the detection and treatment of many non-COVID-19 conditions. Electronic general practice data are a valuable resource which can be used to inform population and individual care decision-making.
This project is based on a collaborative relationship involving the Digital Health Cooperative Research Centre, Macquarie University, Central and Eastern Sydney PHN, Eastern Melbourne PHN, South Eastern Melbourne PHN, South Western Sydney PHN and Outcome Health.
The project will identify emerging trends related to COVID-19, its diagnosis, treatment and medications prescribed, and its impact on patients as well as monitor the impact of interventions/policy decisions. The study will also examine the prevalence of Long COVID and identify strategies for management in Australian general practice.
Ethics approval for this project was granted by Macquarie University Human Research Ethics Committee (Ref No: 5201700872)
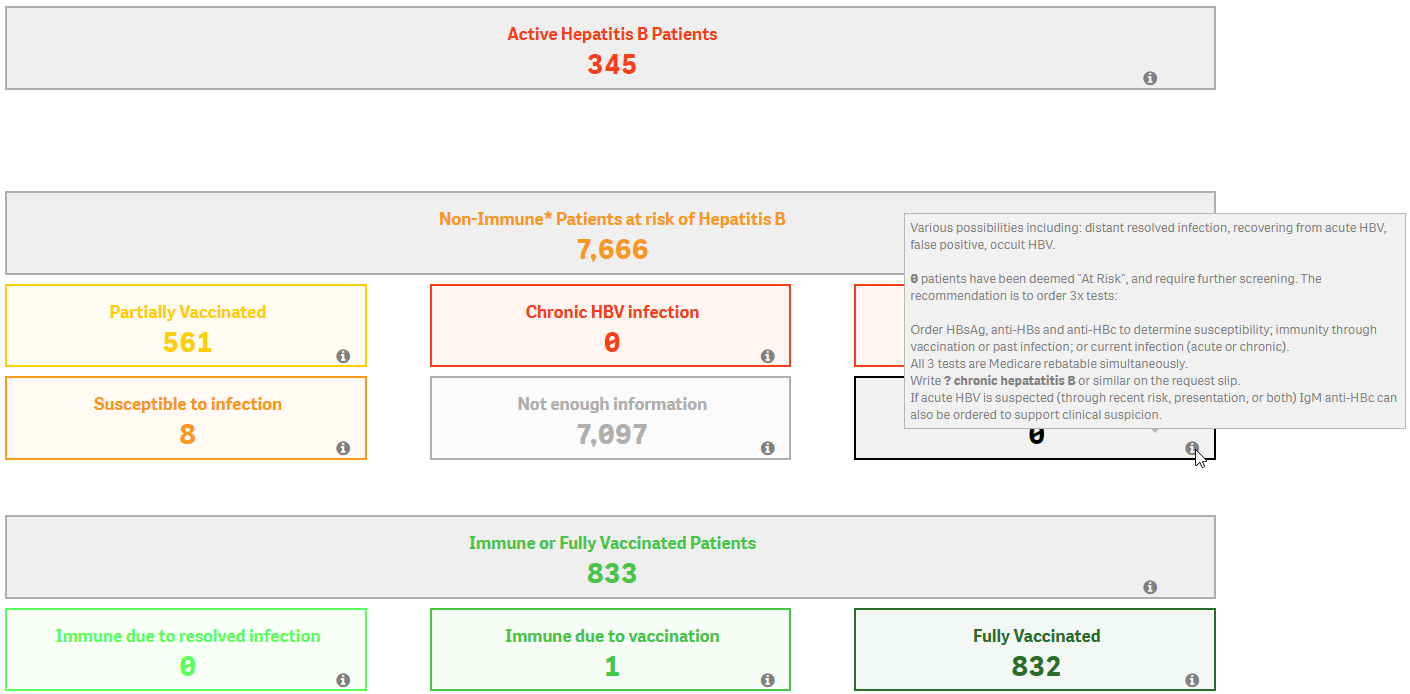
HepLOGIC
This project will design a comprehensive intervention to improve prevention of liver cancer in people living with chronic viral hepatitis. Read more. Ethics approval for this project was granted by Melbourne Health Human Research Ethics Committee (Ref No 2021.231)
SAFESIG GP COVID: Vaccine safety surveillance using de-identified representation data following vaccination
General practice is a critical point of immunisation against COVID19 for a large proportion of the Australian population. This project will benefit GPs, PHNs, the community cared for by them, and the health system by helping to identify unsafe vaccines as early as possible and providing confidence vaccine safety is being closely monitored. Ethics approval for this project was granted by Monash Health Human Ethics Research Committee Ref No RES-18-0000-232A)
Using data to improve outcomes with pharmaceutical opioids
Australia has the 8th highest opioid prescribing rate in the world. Mortality from pharmaceutical opioids has doubled over the last decade. There is an urgent need to better understand opioid use patterns, outcomes and detection of harms. Researchers will use Aurora data to better understand opioid use patterns, identify risk areas around opioid supply and analyse the impacts of opioid-related policy decisions on prescribing. Ethics approval for this project was granted by the Monash University Human Research Ethics Committee (Ref No: 24139)
Primary Health needs and service utilisation of people with disability
Researchers from Summer Foundation (a leading research and support organisation working to increase accessible housing for young people with disability) will lead an exciting project to conduct a three-way privacy-protecting linkage between general practice, the hospital setting and the National Disability Insurance Agency. The primary outcome is to better understand the pattern of health service use by National Disability Insurance Scheme (NDIS) participants and to develop interventions to ensure equitable access to healthcare initiatives by people with disability. Ethics approval for this study was granted by Eastern Health Human Research Ethics Committee (Ref No E20/001/58261)
SNOTWATCH: Establishing impact of common infective conditions at local and community level
Common respiratory and gastrointestinal infections cause significant childhood illness in community, general practice and hospital settings.
The project aims to:
- Create SNOTWATCH- a service mapping respiratory and gastrointestinal results in Victoria for clinicians and consumers to use to see current local activity in their area
- Use these results from the past to estimate the contribution each organism makes in the burden of childhood illness and health-care utilisation. This will help provide the evidence for supporting treatment and vaccine decision making as well as identifying predictable patterns of spread to provide an early warning system for the future.
Ethics approval for this project was granted by Monash Health Human Research Ethics Committee (Ref No RES-19-0000-312A)
The HELP Media Study for Management of Low Back Pain
Low back pain is the leading cause of disability worldwide and in Australia accounts for over $4.8 billion spent on treatments. Patients with low back pain often receive low-value care that is not supported by evidence with a 25% increase in hospitalisations for low back pain in the past 10 years.
This study will trial a media-led intervention that includes evidence-based information on the management of low back pain (LBP), distributed and broadcasted at point-of-care in general practices, to change patient beliefs about LBP. Effectiveness will be measured in terms of patients’ beliefs and attitudes about LBP. Additionally, the study will evaluate the delivery of care at a practice level to determine if the media-led intervention leads to changes in practice (i.e., prescriptions for opioid medication, referrals for medical imaging and Specialists).
The study has ethics approval from Northern Sydney Local Health District Human Research Ethics Committee (Ref: 2022/ETH01928).
SAFER-AUS Trial: Screening for Atrial Fibrillation with ECG to Reduce stroke – a randomised controlled trial
One in four adults aged >40 will develop Atrial Fibrillation (AF) in their lifetime. It is an important health problem associated with a 5-fold increase in stroke, more often disabling or fatal. While AF may give rise to palpitations or other symptoms, there are frequently none, especially in older people with the highest risk of stroke. The primary objective of this study is to determine if screening for AF is effective at reducing stroke (both ischaemic and haemorrhagic) compared to usual care and to quantify other potential benefits and harms of screening. Ethics approval for this project was granted by The University of Sydney Human Research Ethics Committee (Ref No 2021/825)
Publications
A list of publications to date is available here.

“The Outcome Health team has been immensely helpful and insightful around explaining the dataflows and structure of the database, such that WVPHN analysts are already starting to realise new insights not previously possible.”
Manager Health Intelligence & Analytics Western Victoria PHN
Primary Health Networks
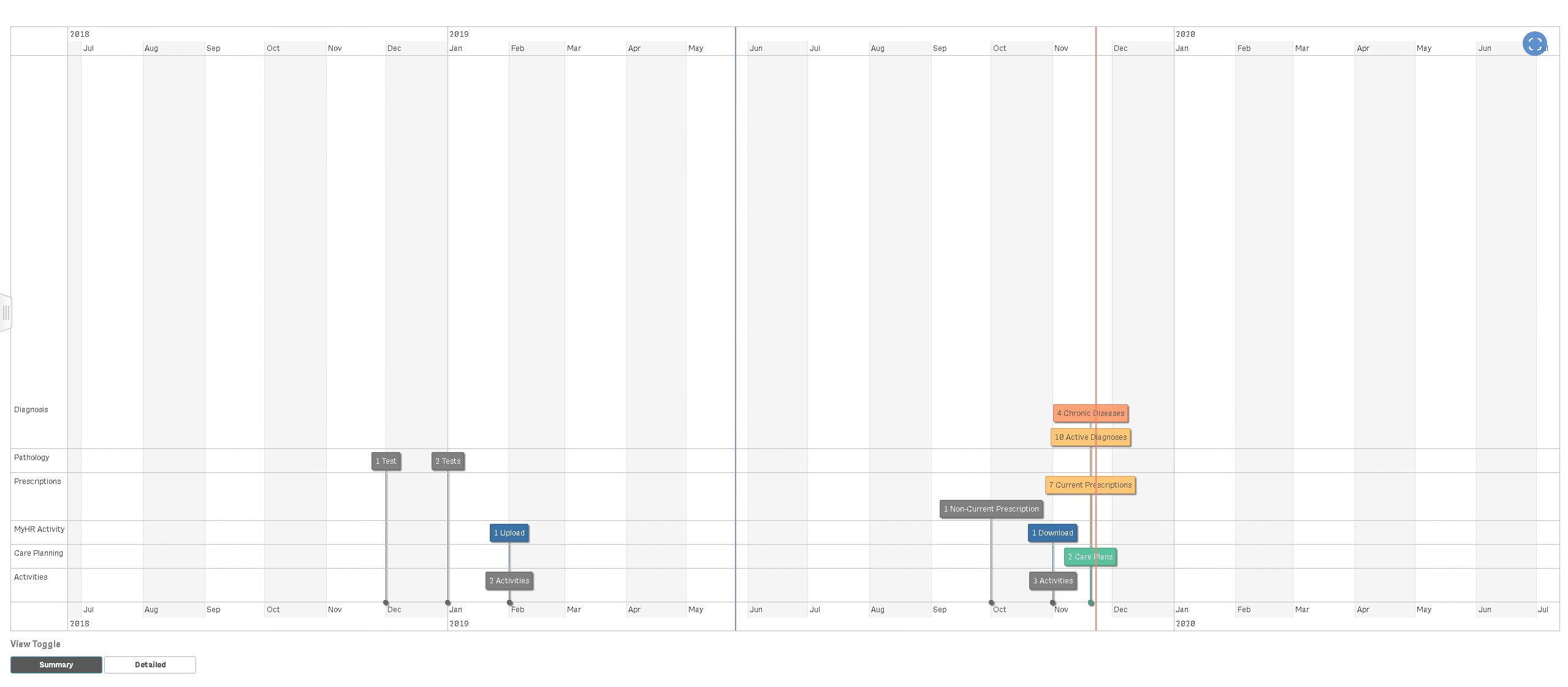
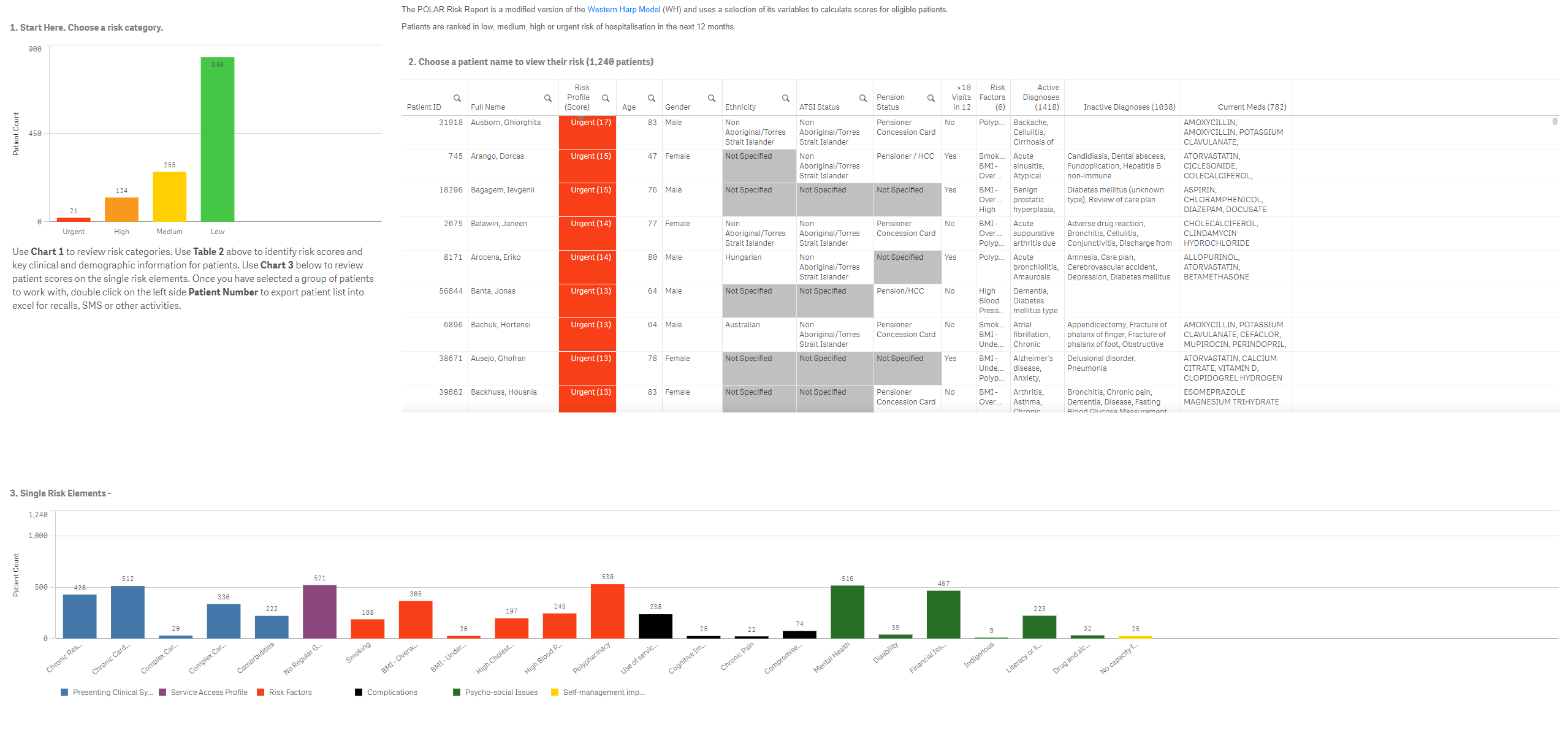
Outcome Health’s POLAR platform provide PHNs easy-to-use tools to visualise and monitor key health and services access trends, providing insights for planning activities, project development, and evaluation.
General Practice
Outcome Health’s POLAR GP is a modern web-based clinical intelligence tool, designed to support GP’s in providing the best patients-focused care, as well as optimising their business output.
Recent Articles
About POLAR – Data Driven Innovation
Outcome Health’s POLAR platform is designed to systemise the benefits of big datasets, and enhance evidence-based decisions that can affect individuals and broad population groups alike.
In a fragmented healthcare system, POLAR provides you with the right solutions to maximise the potential of your data.
Discover our storyStart the conversation
Want to learn more about how POLAR can assist your practice?
We’re ready to connect with you to see how we can help.